- Today I Scoped!
- Posts
- Today I Scoped! #3
Today I Scoped! #3
Issue Three: The (Not So) Silent Hemorrhage
Hi there! 👋
Today I Scoped! is growing beautifully, and I’m happy to hear how much you’re enjoying these stories.
Though, technically, for this one I should probably say “This Week I Scoped!”, because the case was too fascinating to wait.
In this week’s episode, we’re diving into a case that started with hemoptysis and led us into the world of Diffuse Alveolar Hemorrhage (DAH), and, more specifically, pulmonary–renal syndrome. A rare intersection where timing is important, and the line between recovery and irreversible damage can be just hours apart.
Spotlight Procedure
Management of a complex foreign body by Manoj Madhusudan.
To view the entire procedure click HERE.
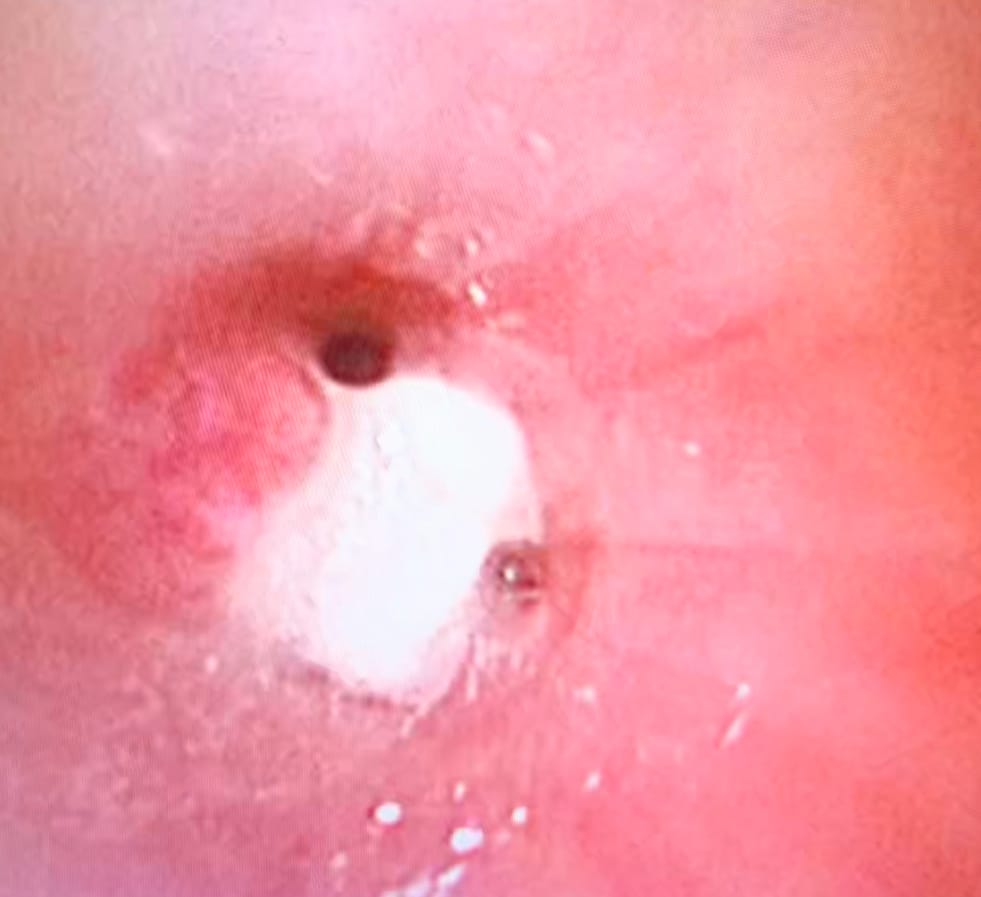
Presentation: A 2-year-old presented with a 2-week history of foreign body aspiration. An initial bronchoscopy removed a fragment, but dense granulation tissue obscured visualization of the distal bronchi, preventing complete retrieval.
Procedure: Given the extent of granulation and limited access to advanced tools such as a cryoprobe, the team initiated systemic corticosteroids to reduce mucosal inflammation. A repeat bronchoscopy at 24 hours was performed.
Outcome: The granulation tissue had markedly regressed, allowing clear visualization of the bronchial tree. A retained fragment in the left upper lobe was identified and successfully removed. The child made an uneventful recovery.
Editor’s Note (M.S.):
Oh, foreign bodies. I believe that whatever you imagine, people will, at some point, aspirate.
Granulations present a unique problem. In most cases, when you successfully remove the foreign body, the underlying inflammation subsides and the granulation will regress naturally.
However, there are critical instances where intervention is necessary: when the granulations themselves cause or exacerbate symptoms, or when the leftover tissue is so large that it effectively behaves like a persistent foreign body, causing obstruction.
To give steroids or not (either systemically or topically via the bronchoscope) is still being debated. But in resource-limited settings, or if you do not have the specialized skills or equipment for removal, I would certainly give steroids a try.
Everyone practicing pediatric interventional pulmonology will encounter severe granulations at some point.
For example, consider our case below, where a peanut obstructed the truncus basalis, causing a massive, reactive granulation that completely obstructed the orifice of the RB7 segment. And yes, I decided to treat the granulation 😅.
P.S. You should definitely follow Manoj. He is not only actively performing IP, but also has a nice publication record worth reading!
DEEP DIVE: The (Not So) Silent Bleeding
This week, I evaluated a teenage boy referred for persistent hemoptysis. He had been previously treated with empiric broad-spectrum antibiotics for a presumed respiratory infection, yet his inflammatory markers remained elevated.
The initial workup revealed an important persitent extra-pulmonary finding: microscopic hematuria with a high yield of Red Blood Cells (RBCs) in the urine sediment. Our planned diagnostic bronchoscopy now had a clear, accelerated mandate.
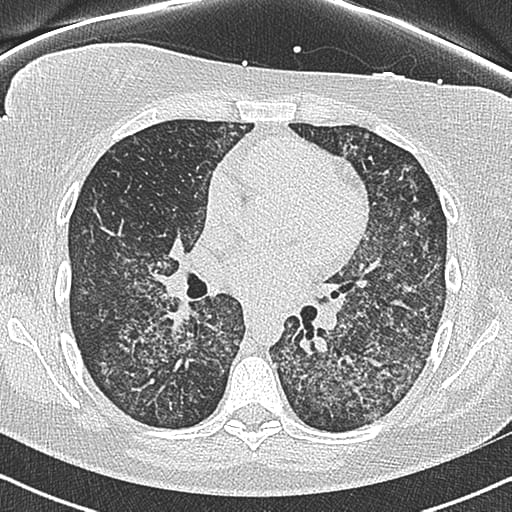
A pre-procedural HRCT confirmed our suspicion, revealing the characteristic diffuse ground-glass opacities bilaterally, signifying active alveolar filling.
Diffuse Alveolar Hemorrhage (DAH)
Pediatric DAH is a life-threatening syndrome characterized by the extravasation of red blood cells from the pulmonary microvasculature into the alveolar spaces. Unlike localized pulmonary hemorrhage, DAH is typically diffuse and leads to acute hypoxemic respiratory failure and profound anemia.
The classic triad of hemoptysis, anemia, and diffuse pulmonary infiltrates is a red flag, but often unreliable in our population. This is why a high index of suspicion, coupled with an interventional readiness, is mandatory.
And in this case, the constelation of hemoptysis and microscopic hematuria presents a textbook example of a pulmonary-renal syndrome.
The Interventional Gold Standard: Bronchoscopy and BAL
The pediatric interventional pulmonologist is central to securing the diagnosis. The goal is to perform a safe, timely procedure to confirm alveolar bleeding and collect high-quality specimens for etiologic workup.
Besides obtaining fluids, we perform bronchoscopy to evaluate the extent of the disease. We want to see if there is a place of active bleeding that can be coagulated.
A. The Progressive Bleeding Rule
BAL in DAH is very interesting!
Definitive confirmation relies on the "Three-Tube Test" of sequential BAL fluid aliquots, instilled into a single, affected subsegment:
Tube 1 (Airway Wash): Primarily reflects upper airway or focal bronchial bleeding.
Tube 2 (Proximal Alveoli): Should show more blood if the source is alveolar.
Tube 3 (Deep Alveoli): The diagnostic criterion for DAH is a progressively bloodier (non-clearing) return across these samples, indicating the source is the diffuse microvasculature.
Our BAL looked like this:

Typical BAL sequence in DAH
B. BAL Specimen Triage
A meticulous specimen collection protocol is non-negotiable and guides the entire treatment plan:
Cytology: Confirm DAH with the percentage of Hemosiderin-Laden Macrophages (HLMs) (typically ≥40% - but the literature is not consistent!). Crucially, in acute, fulminant DAH, HLMs may be absent or low, as it takes 48-72 hours for macrophages to phagocytize the iron.
Infectious Workup: PCR panel for respiratory viruses, bacterial/fungal/mycobacterial cultures, and, if available, consideration of next-generation sequencing (mNGS) in the immunocompromised host.
Flow Cytometry/Cell Count: A high lymphocyte percentage can suggest lymphocytic alveolitis (e.g., in some connective tissue diseases).
C. Airway Management in Acute Bleeding
From our perspective, managing the acutely bleeding pediatric airway under flexible bronchoscopy is a high-stakes procedure:
PEEP Management: Optimal Positive End-Expiratory Pressure (PEEP) can provide a "capillary tamponade" effect, potentially limiting ongoing hemorrhage while providing vital oxygenation.
Airway Isolation: For massive, life-threatening hemoptysis (though less common in DAH than in focal bleeding), the ability to perform selective intubation or balloon blockade (a pediatric interventional skill) to protect the non-bleeding lung is a life-saving measure.
While systemic therapy targets the underlying cause, specific interventional strategies can be considered for rapid hemostasis in severe cases:
Topical Agents (Intrabronchial): For non-life-threatening or localized alveolar bleeding, the direct delivery of adrenaline, or Tranexamic Acid (TXA) via the bronchoscope has been reported in case series, offering local control without the systemic risks (e.g., thrombosis) of IV administration.
Note: Evidence is limited to case reports/series, but the technique is key for the interventional skillset.
Pro tip
BAL is obtained usually from the middle lobe or lingula. But go where the money is. Evaluate the CT scans prior, and observe where the bleeding extent is the highest.
To fully utilize your bronchoscopy skills, lear how to use NBI. NBI, or Narrow-Band Imaging, is used for identifying and treating bleeding in a few ways, primarily by enhancing the visibility of blood vessels during endoscopic procedures. More on that in another newsletter 🙂

NBI image showing a hypervascularized mucosa
Conclusion
Pediatric DAH remains a high-mortality entity, demanding urgent critical care and diagnostic precision. The Pediatric Interventional Pulmonologist is the essential clinician for securing a definitive and timely diagnosis via BAL.
As international collaborative studies continue to refine our understanding, the focus shifts to standardized protocols for the rapid, cause-specific treatment of DAH. Our hyperniche requires us to lead this effort, advocating for early, expert bronchoscopy that can turn a clinical emergency into a treatable condition.
The time spent debating DAH etiology is a luxury we cannot afford, and the interventional pulmonologist must diagnose in real-time to save the lung.
We must always prepare for a massive bleeding, and maintain a clear, unobstructed airway for ventilation, minimize suction-induced trauma, and obtain critical fluid for the ultimate diagnosis.
Once you know how to manage massive hemorrhage, you can call yourself a true interventional pulmonologist.
But managing that true, acute airway-obstructing bleeding is an operational crisis we will save for a future newsletter.
Announcements
How much do you know about Virtual Bronchoscopy and Peripheral Navigation?
We’re developing new content, including a dedicated course, on this underused but powerful diagnostic tool. Stay tuned for updates and early access.

A wonderful view of a tracheal bronchus through real and virtual bronchoscopy
Worthwhile Reading
Floyd Type III Tracheal Agenesis with Laryngeal Cleft and Bronchial Segment Absence: A Case Report published in Pediatric Interventional Pulmonology
Why read: Most of us will never encounter this pathology! Dr. Realista’s group described in detail a patient with Floyd Type III tracheal agenesis, and provided detailed images
✉️ Guest Writers Joining In
Over the past few weeks, several of you have reached out with the idea of contributing as guest writers, and I absolutely love that!
Today I Scoped! was always meant to be a shared space for pediatric interventional pulmonology stories and real-world experiences.
If you've managed an interesting case or have a technique worth sharing, I'd love to feature it. Just send me a short note or draft and we'll polish it for publication.
That’s it for this issue of Today I Scoped! I hope you found something here that you can use in your next case.
Your turn: Have a case, tip, or question worth sharing? Feel free to reply to this email. It might be featured in a future issue.
Of course, feel free to share the newsletter with colleagues who are interested in our field!
Until next time,
Matej